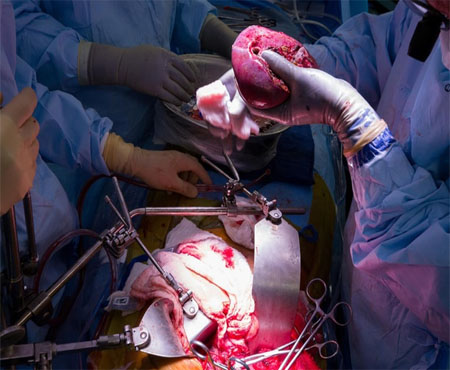
A liver transplant, also known as a hepatic transplant, is the replacement of a diseased liver with a healthy one donated by another person. Being a cure to end-stage liver disease or acute liver failure, it comes with a bunch of several benefits. When you have the end-stage liver disease with no medical therapy being effective, then you may be eligible for a liver transplant. If a patient suffers from a list of prior diseases including Hepatitis B&C, alcoholic liver disease, Wilson’s disease and many more, he/she is eligible for a liver transplant.
In India, more than 80 per cent of live donor liver transplants take place. This is in contrast to the western countries, where approximately 90 per cent of transplants are from deceased donors. Liver Transplant in India costs in the range of USD 33,182 – USD 46,455. India has a very high success rate of Liver Transplant (85-90%) at par with the best in the world. Liver transplant surgeons in India are considered one of the best.
Liver cancer is cancer that begins in the liver cells. The liver is a football-sized organ (the largest) that sits in the upper right portion of the abdomen, beneath the diaphragm and above the stomach. There are six basic types of Liver Cancer. They are Hepatic adenoma, focal nodular hyperplasia (FNH), hepatic angiosarcoma and hemangiosarcoma, hepatocellular cancer, bile duct cancer and Hepatoblastoma, ranging from children to adults.
The hospital stay depends on the surgery done. For Hepatectomy, the hospital stay is approximately six days, with ten days outside the hospital, while 22 days in the hospital and 40 days outside the hospital for a Liver Transplant Surgery. The Liver Cancer Treatment Cost in India ranges between USD 3,982 – USD 5,309 for Liver Resection (Hepatectomy), while Liver Transplant Surgery cost in India ranges between USD 33,182 – USD 46,455.


When your kidneys lose their filtering ability, harmful levels of fluid and waste builds up in your body, which raises your blood pressure and often results in kidney failure. End-stage renal disease happens when the kidneys have lost about 90% of their ability to function normally.A kidney transplant is typically the treatment of choice for kidney failure. But for certain people, a kidney transplant may be riskier than dialysis.The health risks of receiving a kidney transplant include those directly associated with the surgery itself, side effects of taking medications, and rejection of the donor organ.
Although kidney transplantation can treat advanced kidney disease, it is not a cure.The procedure takes around four hours. You should be out of bed in a day or so, and home within a week.According to several studies, 93 per cent of kidney transplants still work at the end of a year and 83 per cent work at the end of 3 years. The cost of transplant varies from USD 6,636 to USD 26,545.
Many people living with RCC don’t experience noticeable symptoms until its later stages. Other less prevalent forms of kidney cancer can also occur such as Wilms’ tumor, which typically occurs in young children.Your treatment options depend on a number of factors, including the cell type and stage of cancer, possible side effects, your preferences and overall health. However, it is most often treated with surgery, targeted therapy, immunotherapy, or a combination of these treatments.
Although every form of treatment for Kidney Cancer carries the risk of side effects, many of them are manageable with the help of doctors.Kidney cancer is typically curable, when detected early and even in more advanced stages, new therapies and treatment methods have led to improved, overall cure rates. The 5-year survival rate for kidney cancer is 75 per cent.


Other areas of surgery also have pediatric specialties of their own that require further training during the residencies and in a fellowship: pediatric cardiothoracic (surgery on the child's heart and/or lungs, including heart and/or lung transplantation), pediatric nephrological surgery (surgery on the child's kidneys and ureters, including renal, or kidney, transplantation), pediatric neurosurgery (surgery on the child's brain, central nervous system, spinal cord, and peripheral nerves), pediatric urological surgery (surgery on the child's urinary bladder and other structures below the kidney necessary for ejaculation), pediatric emergency surgery, surgery involving fetuses or embryos (overlapping with obstetric/gynecological surgery, neonatology, and maternal-fetal medicine), surgery involving adolescents or young adults, pediatric hepatological (liver) and gastrointestinal (stomach and intestines) surgery (including liver and intestinal transplantation in children), pediatric orthopedic surgery (muscle and bone surgery in children), pediatric plastic and reconstructive surgery .
A pancreas transplant is an organ transplant that involves implanting a healthy pancreas (one that can produce insulin) into a person who usually has diabetes.Because the pancreas is a vital organ, performing functions necessary in the digestion process, the recipient's native pancreas is left in place, and the donated pancreas is attached in a different location. In the event of rejection of the new pancreas, which would quickly cause life-threatening diabetes, there would be a significant chance the recipient would not survive very well for long without the native pancreas, however dysfunctional, still in place.
The healthy pancreas comes from a donor who has just died or it may be a partial pancreas from a living donor.[1] At present, pancreas transplants are usually performed in persons with insulin-dependent diabetes, who can develop severe complications. Patients with the most common, and deadliest, form of pancreatic cancer (pancreatic adenomas, which are usually malignant, with a poor prognosis and high risk for metastasis.


Pancreatic cancer arises when cells in the pancreas, a glandular organ behind the stomach, begin to multiply out of control and form a mass. These cancerous cells have the ability to invade other parts of the body. A number of types of pancreatic cancer are known.
The most common, pancreatic adenocarcinoma, accounts for about 90% of cases, and the term "pancreatic cancer" is sometimes used to refer only to that type. These adenocarcinomas start within the part of the pancreas that makes digestive enzymes. Several other types of cancer, which collectively represent the majority of the non-adenocarcinomas, can also arise from these cells. About 1–2% of cases of pancreatic cancer are neuroendocrine tumors, which arise from the hormone-producing cells of the pancreas.These are generally less aggressive than pancreatic adenocarcinoma.
Hepato-Pancreato-Biliary (HPB) surgery is the surgery of the liver, pancreas, and gallbladder. Perhaps the most common presentation under this speciality is jaundice, however there are a wide range of causes for jaundice (in fact, more commonly non-surgical) that every surgical trainee should be aware ofDiseases affecting the gallbladder are common presentations to both primary care and A&E departments. They further will form key differentials in many patients presenting with abdominal pain. Therefore make sure you look over our articles on biliary colic, cholecystitis, and cholangitis.
The phrase “don’t mess with the pancreas” is well known among surgeons due to the severity that pancreatic disease can present with. Pancreatitis can result in severe morbidity and has relatively high mortality rates, therefore knowing its pathophysiology and management is essential. Pancreatic cancer is a condition with a very poor outlook as well, and consequently new treatments are always trying to be developed to improve the survival rates for this disease.
